Breast Cancer Update (2018) —1000 Person Tool, Age 40–49
The Task Force released draft recommendations for breast cancer screening in 2024. The 2011 and 2018 clinical practice guidelines are no longer current. Please click here to view the updated draft recommendations for breast cancer screening.
Updated Task Force Recommendations for Women
For women aged 40–49 years: we conditionally recommend not screening for women who are not at increased risk with mammography
- The balance of benefits and harms is less favourable for women of this age than for older women.
- This recommendation is conditional because some women may wish to be screened as every woman has individual values and preferences and places different importance on benefits and harms.
- If women in this age group wish to be screened, they should have a discussion with their health care provider to decide if screening is best for them.
Who do these recommendations not apply to?
These recommendations don’t apply to anyone at increased risk of breast cancer, such as those with a personal or family history of breast cancer, carriers of specific gene mutations (or who have a first-degree relative with these mutations), or chest radiation therapy before 30 years of age.
What is screening?
Screening is done to attempt to detect potential disease or illness in people who do not have any signs or symptoms of disease.
What is a mammogram?
It is an x-ray of the breast(s) to identify potential cancer.
Why is shared decision making important?
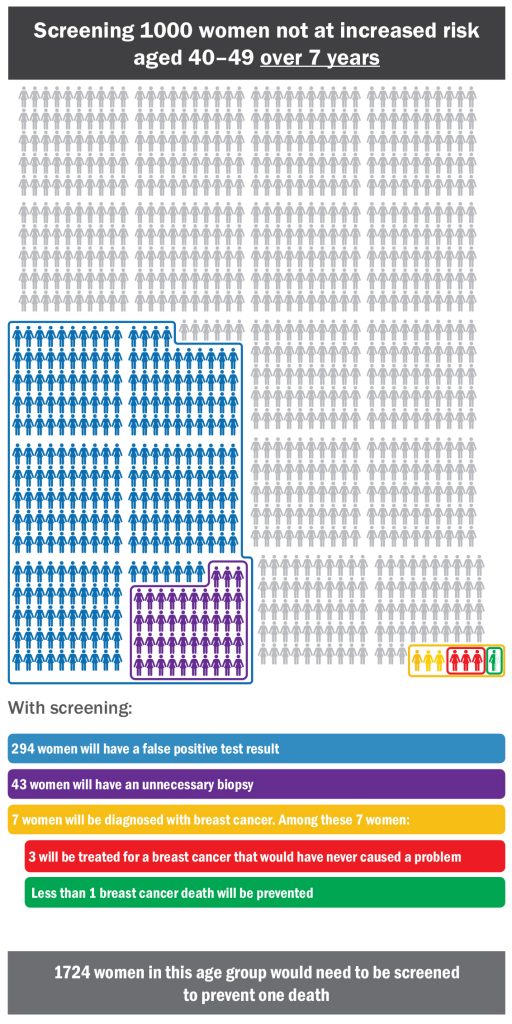
Screening is a personal decision. It is important to weigh the benefits and harms of screening for women in your age group (as shown below) with your health care provider to decide what is best for you.
What are the harms of screening for breast cancer?
Overdiagnosis – Not all breast cancers will cause harm to a woman in her lifetime. With screening, some women will be diagnosed with a cancer that would not have caused them a problem in their lifetime; this is called ‘overdiagnosis’ and leads to unnecessary treatment.
False positives – A false positive test occurs in someone who tested positive (abnormal mammography) but who ultimately is shown not to have cancer. It can lead to additional testing, including biopsy, and may cause psychological and physical harm.
In general, harms of screening are greater in younger women and decrease with age.
What are the benefits of screening for breast cancer?
There is evidence that shows that screening lowers a woman’s risk of dying from breast cancer. In general, the benefits of screening increase with age.
This tool is not a decision aid but is intended to be one step in the shared decision making process.