Breast Cancer Update (2018) —Shared-decision making tool, Age 60-69
The Task Force released draft recommendations for breast cancer screening in 2024. The 2011 and 2018 clinical practice guidelines are no longer current. Please click here to view the updated draft recommendations for breast cancer screening.
*Note: shared-decision making tools require a minor update. These will be updated in early 2023.
Breast Cancer Screening for Women Not at Increased Risk
Guideline Recommendations
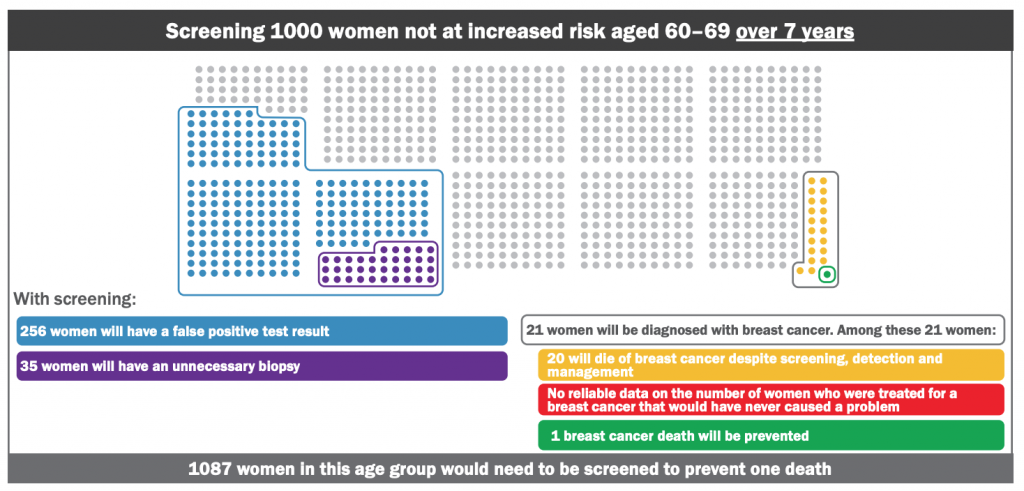
For women aged 60–69 years: we conditionally recommend screening with mammography every two to three years.
- The balance of benefits and harms is more favourable in this group.
- This recommendation is conditional because some women may wish to not be screened if they are concerned about potential harms.
- Women in this age group should have a discussion with their health care provider to decide if screening is the best option for them.
FAQ’s
Who do these recommendations not apply to?
These recommendations don’t apply to women who are at increased risk of breast cancer, such as those with a personal or family history of breast cancer, carriers of specific gene mutations (or who have a mother, sister, or daughter with these mutations), or chest radiation therapy before 30 years of age.
What is screening?
Screening is done to attempt to detect potential disease or illness in people who do not have any signs or symptoms of disease.
What is a mammogram?
It is an x-ray of the breast(s) to identify potential cancer.
Why is shared decision making important?
Screening is a personal decision. It is important to understand and weigh the benefits and harms for women in your age group (as shown below) with your health care provider. This will help you get a better understanding of the issues so that you can decide what is best for you.
| Explanation of benefits and harms |
|---|
| There is evidence that shows that screening lowers a woman’s risk of dying from breast cancer. |
| For you, how important are the following issues? |
| Finding cancer early in hopes of treating sooner than later. |
| Rates |
| 1 life saved per 1000 women screened over 7 years. |
| How important is this benefit/harm to you? |
|
Not Important
○ ○ ○ ○ ○
Very Important
|
| Explanation of benefits and harms |
|---|
| False positives: A false positive test occurs in someone who tested positive (abnormal mammography) but who does not have cancer. It can lead to additional testing, including biopsy, and may cause psychological and physical harm. |
| For you, how important are the following issues? |
| Having follow up tests if you screen positive when there is no cancer present. |
| Rates |
| False positive rate: about 250 per 1000 women screened over 7 years. |
| How important is this benefit/harm to you? |
|
Not Important
○ ○ ○ ○ ○
Very Important
|
| Explanation of benefits and harms |
|---|
| Overdiagnosis: With screening, some women will be diagnosed with a cancer that would not have caused them a problem in their lifetime; this is called ‘overdiagnosis’ and leads to unnecessary treatment (overtreatment). |
| For you, how important are the following issues? |
| Being diagnosed and treated with a cancer that never would have harmed you. |
| Rates |
| No reliable data on overdiagnosis for this age group. |
| How important is this benefit/harm to you? |
|
Not Important
○ ○ ○ ○ ○
Very Important
|
| Explanation of benefits and harms |
|---|
| For you, how important are the following issues? |
| Rates |
| How important is this benefit/harm to you? |
|
Not Important
○ ○ ○ ○ ○
Very Important
|
Any other questions you would like to ask that have not been answered?
What is your decision about screening?
□ I would like to get screened
□ I do not want to get screened
□ I remain undecided