Public – Depression during pregnancy and the postpartum period (2022)
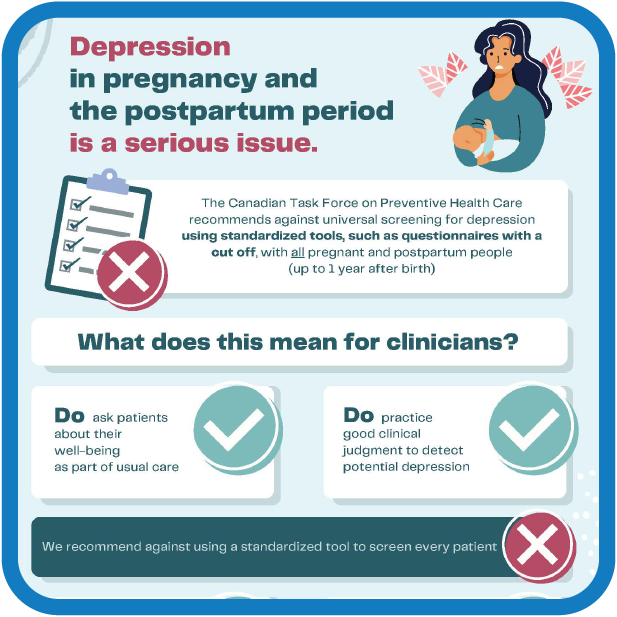
Depression in pregnancy and after giving birth is a serious issue.
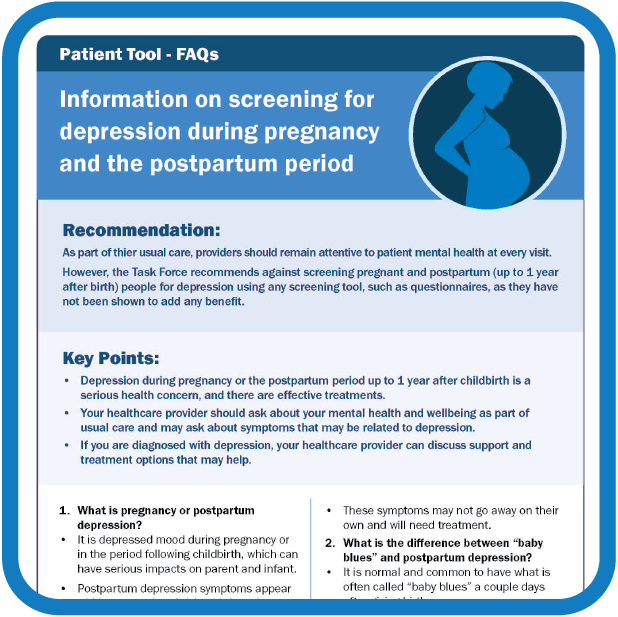
As part of usual care, clinicians should ask pregnant patients and new parents about their mental well-being. However, the Task Force recommends against universal screening for depression using standardized tools, such as questionnaires, with pregnant and postpartum patients (up to 1 year after birth).
Why? The evidence does not show benefit.
For patients
- As part of regular visits, your healthcare provider should ask about well-being. This can include symptoms of depression.
- If you’re worried, talk to your healthcare provider. It’s important to talk to them about any mental health concerns before, during, and after you give birth.
- If you are diagnosed with depression, your healthcare provider can talk about support and treatment options.
“Baby blues” vs. postpartum depression
- It is normal and common to have what’s often called “baby blues” starting a couple days after giving birth.
- These are feelings of sadness, anxiety, and/or being upset with your baby or partner. Other symptoms include unexpected crying, trouble sleeping and loss of appetite.
- “Baby blues” are brought on by a large change in hormones after birth, loss of sleep, and increased stress.
- Symptoms often get better within 1 – 2 weeks without any treatment.
- Postpartum depression shares symptoms with “baby blues”, but it is more intense, lasts longer and needs treatment.
What is screening?
- Screening for depression involves asking a patient a set of questions on a form with answer scores and then acting on them. If your score is high, you’ll get follow-up to see if you are depressed and could benefit from treatment.
- This type of screening hasn’t been shown to improve mental health any more than informal talks between patients and their clinicians about well-being that are part of usual care. It also takes away precious time that could instead be used to talk about mental or physical health.
- This guideline does not apply to pregnant people or those who have given birth in the last year and
- have a history of depression or
- are being assessed or treated for other mental disorders.
Learn more about screening here.
If you’re pregnant or recently had a baby and think you might be depressed, contact your healthcare provider or a depression resource:
- The Canada Suicide Prevention Service
- Quebec: 1.866.277.3553
- Postpartum Support International
- Your Life Counts