Watch Dr. Thériault’s webinar

Task Force Chair and family physician, Dr. Guylène Thériault hosted a webinar on the draft breast cancer screening recommendations to inform stakeholders about the guideline.
Missed it? Watch a webinar which describes how the recommendations were developed and the evidence from the comprehensive review with guidance for clinical practice. The key takeaway is that breast cancer screening is a personal choice. Based on the evidence, the recommendations suggest not systematically screening women 40-49 or women 75+. However, women aged 40 to 74 should be provided information about the benefits and harms of screening to make a decision that aligns with their values and preferences. If someone in aged 40 to 74 is aware of this information and wants to be screened, they should be offered mammography screening every 2 to 3 years.
Watch the webinar here:
Your comments wanted on the new draft guideline
We want to hear from clinicians during the extended public comment period (until August 30th) and ask you to objectively consider the draft recommendations based on the science, including evidence on women’s values and preferences on screening. The comment period is extended to ensure the latest modelling report is available.
By providing feedback, you will help ensure the final guideline is clear and feasible for clinicians to use in practice. We commit to reviewing all responses. Find the draft recommendations here.
Tell us what you think here.
From the front lines
“In a highly emotional and politicized debate, the real question remains: is there a benefit to starting breast cancer screening at age 40 vs. at age 50 for women at average risk?
Thanks to modelling, the Task Force was able to answer this question, with a result of just under 1 breast cancer death prevented per 1,000 women screened. What the guidelines also have the merit of doing is presenting the risks associated with screening in a factual manner. This is because there are harms: unnecessary and anxiety-provoking additional investigations, biopsies, and overdiagnosis. These harms were graphically represented by the Task Force to enable women aged 40 to 50 to make an informed choice.
Therefore, the Task Force’s final recommendation is not to discourage screening (as has unfortunately been heard) but rather to share the decision with the patients, taking into account each individual’s values and preferences. These recommendations are based on a rigorous scientific process led by a family physician qualified in evidence-based medicine who surrounded herself with a diverse team and patient partners.
Do you want to debate with the group? The recommendations are provisional and open for comments extended until August 30, 2024.
Do so using rational, factual, and scientific arguments. Because if we let emotions and politics enter into every scientific discussion, we risk making very poor choices.”

– Dr. Mathieu Pelletier, family physician, Saint-Charles-Borromée, Quebec
Translation and excerpt from Dr. Pelletier’s blog in Profession Santé (Medical Post subscription required).
Get the facts
“What are the potential harms of screening?”
Harms of screening include additional tests such as imaging or biopsies (formerly called false positives), and overdiagnosis, which means finding and treating a cancer that was never going to cause harm in the person’s lifetime.
The evidence showed that for 1000 women screened in their 40s over 10 years
- About two of them will be overdiagnosed
- 368 will undergo additional tests
- 55 will have biopsies to confirm no cancer
The evidence also found that less than one death from breast cancer would be prevented over 10 years in this group. As for any benefit from less harsh treatment, we relied on modelling. See the discussion tools for more information.
Information like this on benefits and harms is needed by patients so that they can decide if screening is right for them.
Find more information on benefits and harms from the draft recommendations here.
“What evidence did you include in the recommendation?”
For women at average or moderately increased risk of breast cancer, we asked the following:
- What are the benefits and harms of breast cancer screening in women 40 and older?
- Age to start and stop screening and the use of different screening tests and time between screenings
- What are the values and preferences of women towards breast cancer screening?
Evidence to address these questions included:

For these recommendations, we included:
- 92 observational studies
- 1 modelling study
- 16 randomized controlled trials
- 82 patient values and preferences studies
- Statistics Canada and Canadian jurisdictional data
- Contextual information on racial disparities (28 observational studies)
We conducted analyses with and without the Canadian National Breast Screening Study. Consistent with other groups (e.g., USPSTF), findings from the systematic review showed no substantial differences in mortality results with or without this study.
Facts about the draft guideline
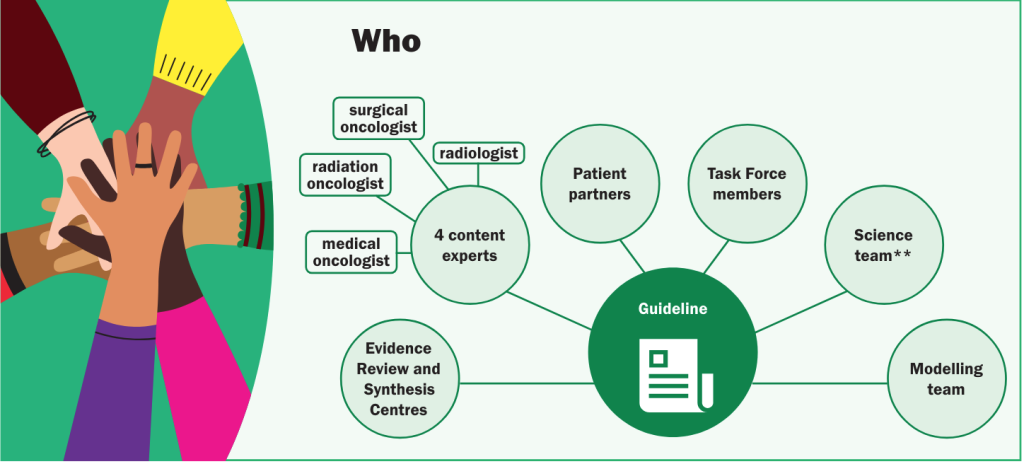
The draft recommendations were developed by Task Force members who are family physicians, nurse practitioners, specialists and methods experts with expertise in primary care, evaluating evidence, and the development of preventive care guidelines. In addition,
- Four specialists (a medical oncologist, a radiation oncologist, a surgical oncologist, a radiologist) and three patient partners were on the working group and involved in every step in gathering the evidence to inform the draft recommendations.
- Two Evidence Synthesis Review Centres and scientific staff helped develop the draft recommendations.
Read the draft recommendations here.
Clinician tools
Patient tools for primary care
Use our tools to help patients aged 40-74 understand the benefits and harms of breast cancer screening.
Next up: absolute vs. relative risk, recommendations for dense breasts and more

