Your comments wanted on the new draft guideline
Breast cancer is a disease that touches many Canadians, and we all want to find ways to reduce the burden of this illness.
This spring, the Canadian Task Force on Preventive Health Care (Task Force) unveiled updated draft breast cancer screening recommendations, following a comprehensive evidence review. We understand that the draft recommendations may be surprising to some, and we ask health care providers to objectively consider them based on the science, including evidence on women’s values and preferences on screening. Find the draft recommendations here.
We want to hear from clinicians during the public comment period ending July 11. By providing feedback, you will help ensure the final guideline is clear and feasible for clinicians to use in practice. We commit to reviewing all responses.
Tell us what you think here.

From the front lines
“Navigating the concerns of women patients, and helping them choose among the different guideline recommendations, is difficult. For me, the Canadian Task Force is the most useful because it emphasizes a woman’s choice, and provides clear discussion aids for each age group to help women choose. The tools clearly identify the small size of the likely benefit and the potential harms in ways that people can understand.
The Task Force also clearly identifies what we do not know, so that we can all work on filling those gaps in future.”
– Dr. J. Dickinson, family physician, Calgary
Get the facts
What is the evidence on the benefits and harms?
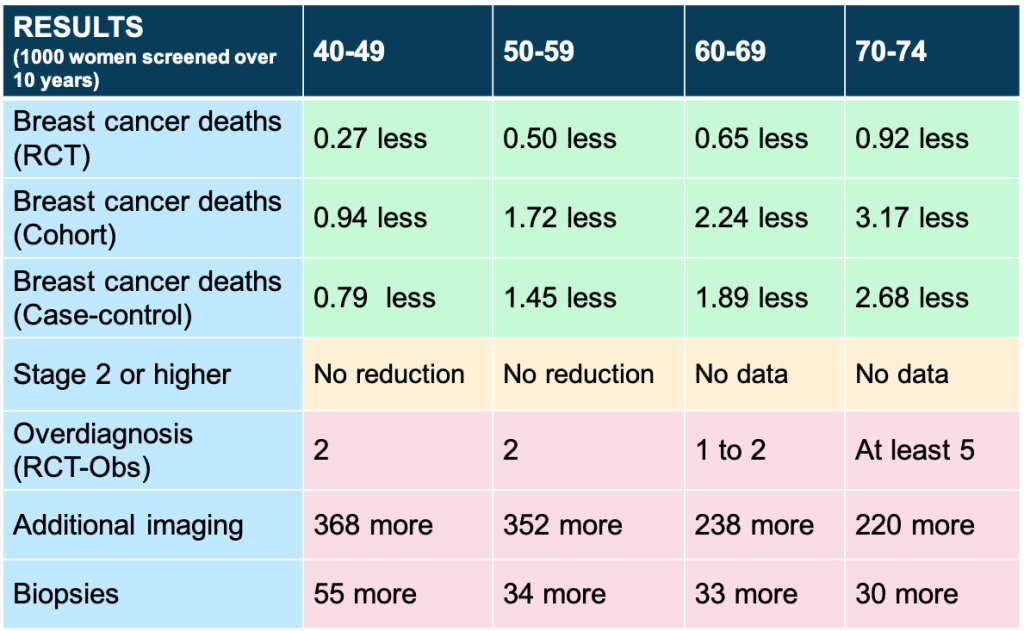
This table shows the benefits and harms of breast cancer screening for ages 40-74 in absolute numbers per 1000 people over 10 years
What is the evidence on women’s values and preferences by age?
Ages 40-49 – The evidence review on values and preferences showed that a majority of patients may not weigh the benefits as greater than the harms. However, all sources of information, including patient partners/clinical expert feedback, demonstrated variability in patient values and preferences.
Ages 50-74 – The evidence review on values and preferences showed that a majority of patients may weigh the benefit as greater than the harms. However, all sources of information, including patient partners/clinical expert feedback, demonstrated variability in patient values and preferences.
What are the draft recommendations by age?
Ages 40-49 – Based on the current evidence (trials, observational studies, modelling and a review on values and preferences), we suggest not to systematically screen with mammography. Because individual values and preferences may differ, those who want to be screened after being informed of the benefits and harms should be offered screening every 2 to 3 years. (conditional recommendation, very low certainty)
Ages 50-74 – Based on the current evidence (trials, observational studies modelling and a review on values and preferences), we suggest screening with mammography every 2 to 3 years. Because individual values and preferences may differ, it is important that women aged 50 to 74 have information about the benefits and harms of screening to make their decision (conditional recommendation, very low certainty)
Ages 75+ – Based on the current evidence (observational studies and modelling; no trials available), we suggest not to screen with mammography (conditional recommendation, very low certainty).
Why are the recommendations conditional?
The Task Force makes conditional recommendations when:
- there is a close balance between benefits and harms, or
- we are uncertain about the benefits and harms, and
- there is variation in patient preferences.
Because there are harms with breast cancer screening that must be balanced with benefits, and important variability in patient values and preferences, the Task Force recommendation is conditional.

Therefore, people aged 40 to 74 should be provided information about the benefits and harms of screening to make a decision that aligns with their values and preferences. If someone in this age range is aware of this information and wants to be screened, they should be offered mammography screening every 2 to 3 years.
Because of the very low certainty of the evidence, we are calling for more research.
Clinician tools
Patient tools for primary care
Next up: how we developed the draft guideline, clinician tools and more

