In the news

We understand that the draft breast cancer screening guideline may be surprising to some. Sometimes the scientific process reveals facts that contradict mainstream thinking, and we know this may be one of those times.
A Medscape article recently explored our process for developing the guidelines, along with the facts about breast cancer including the benefits and harms of screening. The article featured Task Force Chair Dr. Guylène Thériault, along with comments from other medical professionals and breast cancer experts. Read the full article here.
We want your feedback on the draft guidelines
We want to hear from clinicians during the public comment period, now extended to August 30. We ask you to objectively consider the draft recommendations based on the science, including evidence on women’s values and preferences on screening.
By providing feedback, you will help ensure the final guidelines are clear and feasible for clinicians to use in practice. We commit to reviewing all responses. Find the draft recommendations here.
From the front lines
A time to screen and a time to talk first.
Could these two statements be true at the same time? The CTFPHC, comprised of volunteer members from multiple disciplines, has released updated breast cancer screening guidelines (2024) based on available research, which differ from the USPSTF. The CTFPHC’s breast screening guidelines suggest a strong evidence approach with shared decision-making (SDM) for women aged 40-49. The USPSTF suggests a strong advocacy approach with direct to screen, no SDM.
As a family doctor, educator and faculty developer, I have an interest in prevention and screening, best outcomes for patients, and how to teach effective and responsible screening to medical learners. I understand that screening is complex! As a woman I know making health decisions can be difficult and feel strongly that health care should NOT be weaponized. Women need information to choose. Medical learners need to understand the nuances in choosing wisely. Health care providers need to understand both population health and how to adapt it appropriately to individual patients.
The CTFPHC’s breast screening guidelines encourage both the patient and family doctor to discern between the time to screen and the time to talk first. Amongst the screening uproar, I hold on to two truths. First, I am grateful for the preventive health screening in Canada and want it to get to the right people at the right time. Second, with all humility, I understand screening recommendations can and have been incorrect in the past (e.g., annual PAPs starting when sexually active). The best I can do as a health care provider is incorporate a patient-centered approach. Combine available evidence and advocacy and include the patient in the discussion.

– Viola Antao MD, CCFP, MHSc, FCFP
Associate Professor
Mentorship Lead
Temerty Department of Family & Community Medicine
University of Toronto
Get the facts
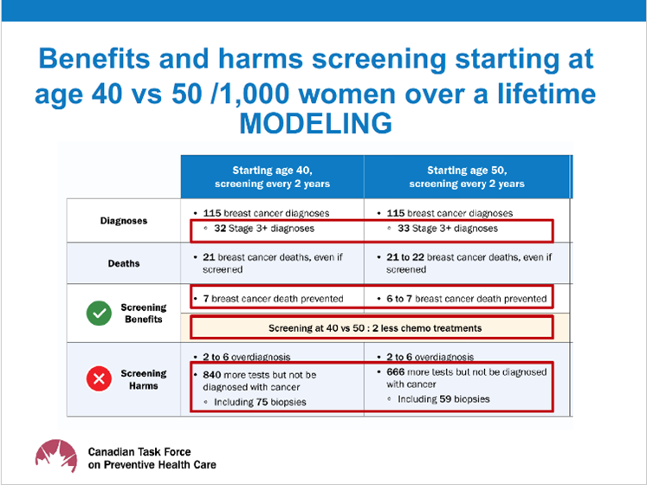
What are the estimated lifetime benefits and harms of starting to screen at 40 vs 50?
We looked for information on how screening can decrease advanced stage cancer (Stage 3+) if we started at age 40 vs 50. As there was almost no data, we had to rely on modelling. The OncoSim-Breast microsimulation model estimated benefits and harms, including reductions in advanced cancer, over a lifetime comparing systematic screening starting at age 40 versus 50 years. The model assumed that 100% of eligible people participate and adhere to screening every 2 years.
While we understand the results are surprising, the modelling data showed that the difference in Stage 3+ cancers was 1 per 1,000 women over a lifetime. Other benefits and harms were also similar. See the figure below.
We also reviewed modelling analyses on other benefits and harms of breast cancer screening with digital mammography using different ages to start and stop screening and screening intervals. Stay tuned for an update of those numbers when the OncoSim model will be rerun with the most up-to-date estimates. (See the draft recommendations here for the detailed information).
What are the screening recommendations for women with dense breasts?
For those who have been identified as having dense breasts, we did not find any evidence on the benefit of supplemental screening (i.e., mammogram followed by ultrasound or MRI) for outcomes important to patients (e.g., stage at diagnosis, death). Therefore, we do not suggest the use of MRI or ultrasound as supplementary screening tests for people with dense breasts. The balance of benefits and harms is unknown.
If interested in screening, women who know that they have increased breast density (Category C and D) should refer to recommendations that correspond to their age group.
Clinician tools
Patient tools for primary care
Use our tools to help patients aged 40-74 understand the benefits and harms of breast cancer screening.
Next up: Understanding relative vs. absolute risk, overdiagnosis and more.